Request a Referral
* View our call center hours
Please visit our privacy policy for more information.
Innovating Heart Failure Care: Double-VAD Procedure Creates Working Artificial Heart
Emory heart failure patient is one of three in the nation to live at home with a total artificial heart
An Emory Healthcare patient with severe end-stage heart failure is one of only three people in the nation to live a normal life at home with a total artificial heart, thanks to a groundbreaking procedure by a surgeon at Emory University Hospital.
Emory is one of only a few hospitals in the country that can perform this very complex procedure.
Redefining options beyond heart transplant
For patients with end-stage heart failure, a heart transplant is the optimal treatment, but the wait for a compatible heart can be lengthy.
In the interim, patients with left ventricular heart failure can survive with mechanical support in the form of an implanted left ventricular assist device (LVAD). Alternatively, those with a compromised right ventricle can live with a right ventricular assist device (RVAD).
For the 10 to 15% of severe heart failure patients with biventricular failure, in which both the left and right sides of the heart are too weak to function, however, there no long-term options other than a transplant.
Mani A. Daneshmand, MD, cardiac surgeon and chief of Thoracic Transplant and MCS Surgery at Emory, has given hope to these so-called “orphaned” patients with a custom biventricular support system.
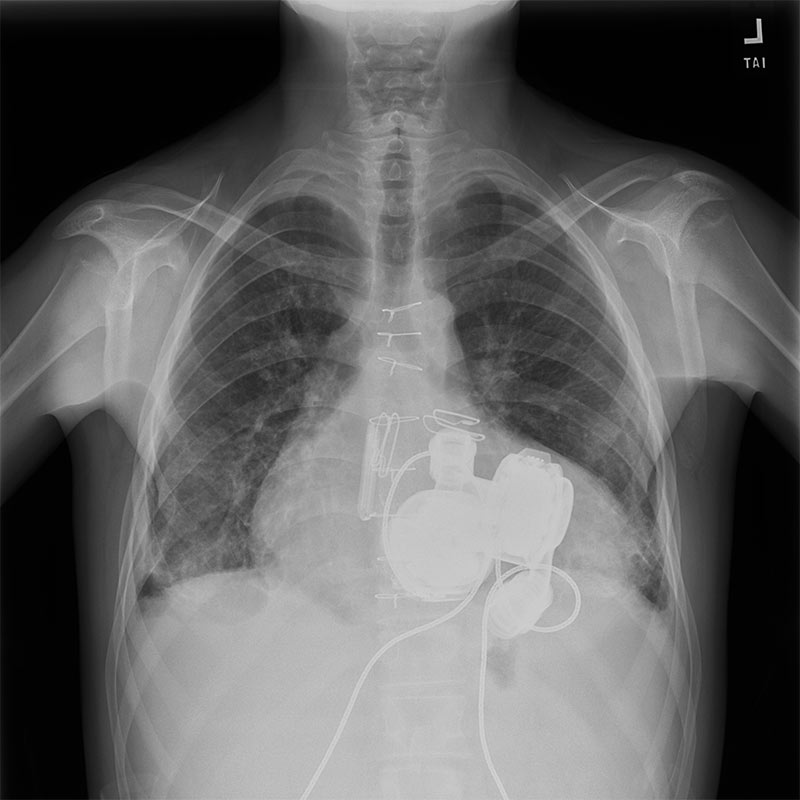
The HeartMate 6 (HM6) involves surgically implanting two commercially available HeartMate 3 (HM3) pumps — one configured as an LVAD and one as an RVAD — to function as a total artificial heart.
Congenital heart condition becomes life-threatening
An 18-year-old male was referred to Emory University Hospital from Children’s Healthcare of Atlanta. Born with congenital aortic stenosis, he had undergone an aortic valve repair using the Ross procedure, which replaced his failing aortic valve using a homograft (a donor pulmonic valve) for the pulmonic position.
Although he was stabilized for a while, his heart function never fully normalized and steadily deteriorated over time.
The patient eventually experienced a crisis when acute exacerbation of systolic heart failure landed him in the emergency room. His condition quickly escalated to cardiogenic shock, requiring immediate, maximum life support. Extracorporeal Membrane Oxygenation (ECMO) stabilized him while his care team at Children's Healthcare of Atlanta explored the possibility of a heart transplant.
A custom solution when there is a barrier to heart transplant
The transplant workup revealed that the patient had a rare barrier to transplant, having developed powerful antibodies against Human Leukocyte Antigens (HLA), most likely in response to the prior surgery and homograft.
These results indicated that he would likely reject over 99% of all potential heart donors in the United States. This made a timely, standard heart transplant impossible.
Upon transfer to Emory University Hospital, Dr. Daneshmand and his team confirmed the patient’s ineligibility for a transplant. His only option for survival was to implant the HM6 system. After counseling the patient and his family about the potential for death during or immediately following the procedure, and a prolonged, difficult recovery, they chose to proceed.
Inside the double-VAD procedure
First, Dr. Daneshmand began by reopening the patient’s chest to access his heart.
Then, the surgical team then initiated cardiopulmonary bypass (a heart-lung machine) before systematically removing the failing native heart structures — the left and right ventricles, and the pulmonary and aortic valves.
Then, the surgical team then initiated cardiopulmonary bypass (a heart-lung machine) before systematically removing the failing native heart structures — the left and right ventricles, and the pulmonary and aortic valves.
A robust, double-layered Dacron graft was sewn to the inflow points: the mitral annulus, for blood from the lungs to the LVAD and the tricuspid annulus for blood from the body to the RVAD. To prevent future bleeding, all remaining heart muscle and tissue were carefully oversewn in two protective layers.
The two HM3 pumps were then implanted. Their inflow cannulas were secured to the Dacron grafts, while the outflow grafts were connected to the major arteries: the left-sided pump to the aorta (end-to-end), and the right-sided pump to the pulmonary artery.
Overcoming post-surgical complications
Following implantation, a complication arose as the patient’s lungs, damaged by the weeks on ECMO, began to fill with fluid upon receiving normalized blood flow. The team quickly converted his support to veno-venous (VV) ECMO, a circuit used exclusively for lung support.
The final step involved placing a tissue expander preventing the chest cavity from collapsing. Since the two VAD pumps are significantly smaller than the native heart, the mediastinum would shrink, compromising a potential future transplant. A tissue expander was placed to keep the space open before the chest was closed.
Life after surgery
The patient stayed in the hospital for the four-month recovery period. The immediate goal was lung recovery, followed by extensive physical and mental rehabilitation. Due to his more than 6 weeks in bed on the ECMO prior to the procedure, regaining strength was a protracted process.
The patient ultimately achieved a full functional recovery. Today, he leads a normal, active life.
Restricted only from swimming due to the external drivelines and batteries he carries constantly. His follow-up visits have transitioned from weekly to a routine of approximately once a month.
Due to his high sensitization, the team is considering the highly complex HALT-D (Heart After Liver Transplant with Domino) strategy — a combined heart and liver transplant from the same donor. The transplanted liver acts as a "sponge" to rapidly destroy the donor-specific HLA antibodies in the bloodstream, allowing the new heart to be placed shortly after without acute rejection risk.
About Emory Heart & Vascular
Emory Heart & Vascular is nationally recognized for its depth of expertise in cardiovascular care. From routine care to complex cases, our teams deliver advanced therapies shaped by research, innovation and real-world collaboration.
Refer a patient to an Emory heart failure specialist
Please call our physician referral line at 404-778-5050
Request a Referral
* View our call center hours
Please visit our privacy policy for more information.
Request a Referral
* View our call center hours
Please visit our privacy policy for more information.