Elberta Jenkins’ cardiologist delivered the news compassionately but directly. There was nothing else he could do for her. Jenkins had undergone a triple bypass in 2008 following a heart attack, but now, in 2020, two of the four main valves in her heart were failing. She needed another open-heart surgery, but she was no longer a candidate due to her age.
“I remember feeling hopeless,” says Jenkins, who is now 82. “But then my doctor said that even though he had run out of options for me, his former instructor and mentor, Dr. Greenbaum, was practicing in Atlanta, and he might be able to help me.”
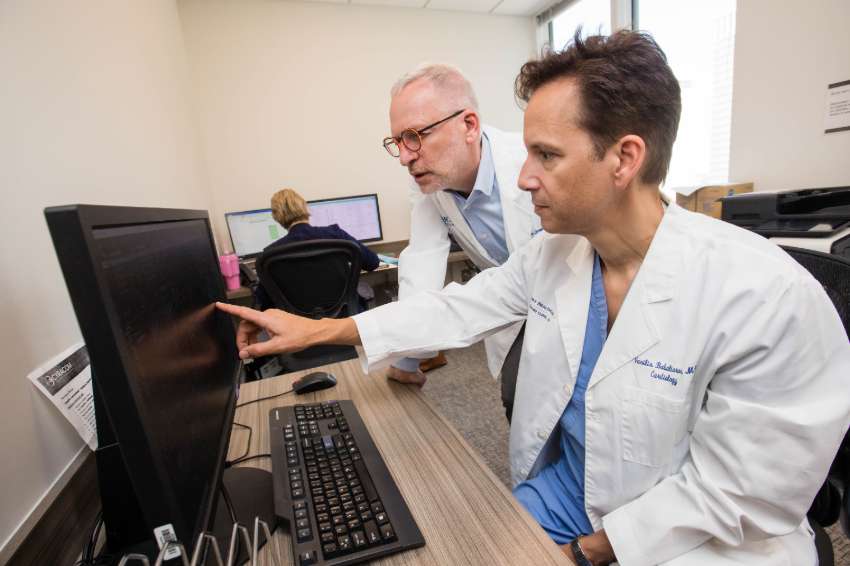
That’s how Jenkins found her way from Orange Park, Florida, to the offices of Adam Greenbaum, MD, and Vasilis Babaliaros, MD, at the Structural Heart & Valve Center at Emory University Hospital Midtown. Greenbaum immediately recognized Jenkins as a good candidate for a noninvasive procedure Emory had helped pioneer, which he used to replace her aortic valve via a catheter. He hoped the new valve would give Jenkins the relief she needed.
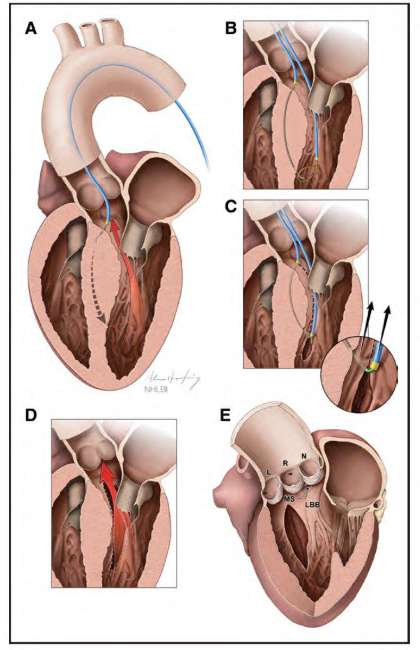
It did not. She still suffered from the deterioration of another main valve in her heart, the mitral valve, which controls the blood flow from the lungs into the heart. She also had hypertrophic cardiomyopathy — a condition characterized by an overly large and stiff heart muscle. These conditions in combination greatly reduced the blood flow from Jenkins’ heart, and the enlarged muscle also blocked the space needed for a new mitral valve.
“She kept getting worse,” says Meri Pyle, Jenkins’ daughter who accompanied her mother on her doctors’ visits. “She got to the point where she could only walk a few steps before she’d have to sit down and rest. She started staying in bed, and she told me she just didn’t want to live like that.”