Turning 50 is a big milestone for many people — a lot happens in a half-century, after all, including major medical and technological advancements. And for some time, reaching age 50 has been associated with having your first colonoscopy.
But doctors today will tell you: when it comes to your colonoscopy, 45 is the new 50. Why the shift?

Sonali Sakaria, MD, is the Emory Clinic clinical chief of gastroenterology (GI) at Emory Decatur Hospital and completed her internal medicine and gastroenterology training at Emory University School of Medicine. "Colorectal cancer is the third leading cancer in men and women equally and the second leading cause of cancer death," she says. "Recent studies have highlighted an increased incidence of colorectal cancer in individuals younger than age 50.”
With rising numbers of colorectal cancer, national health guidelines have changed. In 2018, the American Cancer Society revised its guidelines to recommend a first screening for colon cancer at age 45 — or earlier if you have a family history. In 2021, the U.S. Preventive Services Task Force (USPSTF) updated its recommendations to match the American Cancer Society’s guidelines, lowering the age of first screening to 45.
How do colonoscopies prevent colorectal cancer?
Colorectal cancer is preventable — and it’s treatable when caught early. In fact, colon cancer screening is one of the most effective early detection and prevention services available in medicine today.
Since 2011, Sakaria explains, the rate of colon cancer has increased by roughly 1% each year in patients both under and over age 50. Modeling studies, which are simulations run using available data to make predictions, have shown that starting colonoscopies at age 45 would help save lives. During screening, it’s possible to remove polyps early — if pre-cancerous polyps are removed, they won’t turn into colon cancer later.
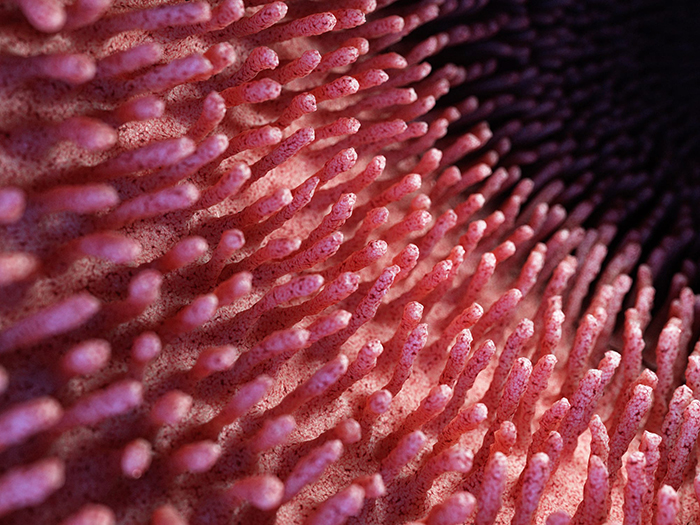
One of the things doctors may detect during colonoscopies are polyps — tissue growths in the colon or rectum that may be benign or cancerous. During a colonoscopy screening, polyps are removed and then tested. If pre-cancerous polyps are removed early, they won’t turn into colon cancer later — one of the biggest benefits of colonoscopies.
“It’s a screening test that’s as important as getting pap smears, mammograms and prostate cancer screening. It truly does save lives,” Sakaria says. “I think educating patients on how the procedure is done alleviates a lot of their concerns. And the more educated patients are, the more likely they are going to be willing to undergo the screening procedure.”
In addition to regular screenings like colonoscopies, the National Cancer Institute recommends the following colorectal cancer prevention guidelines:
- Not smoking
- Drinking in moderation or not at all
- Maintaining a body mass index below 25
- Being physically active every day
At Winship Cancer Institute of Emory University, clinical trials and research are under way to explore more options for colorectal prevention. Some examples of prevention-related research include:
- How the genomic makeup of individuals diagnosed with cancer prior to age 50 differs from older patients
- Whether or not fiber-rich foods are effective at treating obesity and preventing colorectal cancer
- The effect certain chemotherapy drugs have on reducing patients’ risk of colorectal cancer recurrence